In a post based on a recent talk, Siân Harris shares some of what we have learned from the first four years of involving a patient advisory group in non-clinical cancer research in the Integrative Cancer Epidemiology Programme. (more…)
Category: cancer
Away day brings programmes together to explore cancer challenges
Bringing researchers from different areas together is vital in sharing expertise and generating opportunities for new collaborations and connections. Last week members of the Integrative Cancer Epidemiology Programme (ICEP) joined colleagues specialising in Mendelian randomization (MR) within the MRC Integrative Epidemiology Unit (IEU), for a day of discussion, networking and sharing their latest research.
Here, Senior Research Fellow Philip Haycock, who leads the Cancer Progression and Drug Target research theme in ICEP, summarises some the day’s discussions and overlapping research. (more…)
Adiposity in childhood affects the risk of breast cancer by changing breast tissue composition, study suggests

Breast cancer is the most common cancer in women worldwide. With rates continuing to rise, there is an urgent need to identify new modifiable breast cancer risk factors. New research led by the University of Bristol suggests that higher adiposity in childhood leads to less dense breast tissue forming, which results in a reduced breast cancer risk. However, further research is needed to understand the mechanism of the overall protective effect of childhood adiposity to identify new targets for intervention and prevention. (more…)
World Cancer Day – An interview with Professor Richard Martin discussing interdisciplinary cancer research
Richard Martin was interviewed by Caroline Bull, Associate Editor of PLOS ONE, in a post that was first published on the EveryONE blog.
World Cancer Day, held every 4 February, is a global initiative led by the Union for International Cancer Control (UICC) to raise awareness, improve education and catalyze action. This year’s theme is ‘Close the Care Gap: Uniting our voices and taking action’.
Each year, PLOS ONE publishes more than 1000 cancer-related research articles from authors across the globe. In celebration of this year’s theme, we interview PLOS ONE author Richard Martin, Professor of Clinical Epidemiology at the University of Bristol and co-lead researcher of the Integrative Cancer Epidemiology Programme. We ask how Open Science can contribute to interdisciplinary cancer research and how engagement with patient communities has increased the impact of their research. (more…)
Helping the public explore key health questions
By Emma Hazelwood and Amy Campbell
‘What do you think is most important for our health – our genetics or the environment we live in; nature or nurture?’
This was a key question that we posed to members of the public as part of a roundtable discussion on the topic of “Inherited Health”. We hosted our roundtable as part of the recent FUTURES public engagement festival and our event was attended by approximately 25 members of the public including retired professors, patent lawyers, and civil servants. (more…)
How can your gut microbiome affect risk of cancer?
1 Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, BS8 2BN
2 Medical Research Council (MRC-IEU), University of Bristol, Bristol, BS8 2BN
3 Cancer Research UK (CRUK) Integrative Cancer Epidemiology Programme (ICEP), University of Bristol, Bristol, BS8 2BN
The causes of cancer are often preventable
Cancer, a disease that has a profound impact on the lives of individuals all over the world, also has an ever-increasing burden. And yet, evidence indicates that over 40% of all cancers are likely explained by preventable causes. One of the main challenges is identifying so-called ‘modifiable risk factors’ for cancer – aspects of our environment that we can change to reduce the incidence of disease.
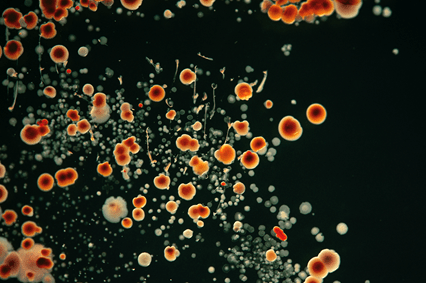
The gut microbiome could influence cancer risk
The gut microbiome is a system of microorganisms that helps us digest food, produce essential molecules and protects us against harmful infections. There is growing evidence supporting the relationship between the human gut microbiome and risk of cancer, including lung, breast, bowel and prostate cancers. For example, experiments have shown that changing the gut microbiome (e.g., by using pre- or pro-biotics) may reduce the risk of developing colorectal cancer. Research also suggests that people with colorectal cancer have lower microbiota diversity and different types of bacteria within their gut compared to those without a diagnosis.
As the gut microbiome can have a substantial impact on their host’s metabolism and immune response, there are many biological mechanisms by which the gut microbiome could influence cancer development and progression. However, we don’t yet know how the gut microbiome can do this.
Human studies in this context have used small samples of individuals and measure both the microbiome and disease at the same time. These factors can make it difficult to tease apart correlation from causation – i.e., does variation in the gut microbiome change someone’s risk of cancer or is it the existence of cancer that leads to variation in the gut microbiome? This is an important question because the main aim of such research is to understand the causes of cancer and how we can prevent the disease. We want to fully understand whether altering the gut microbiome can reduce the burden of cancer at a population level or whether it is simply a marker of cancer itself.
I’m inviting feedback on your knowledge and understanding of the gut microbiome and cancer – please take this 5-minute survey (click here for survey) to contribute your thoughts.
People are interested in their gut microbiome
Even though we don’t yet know much about the causal relevance of the gut microbiome, there is still a growing market for commercial initiatives targeting the microbiome as a consumer-driven intervention. This usually involves companies obtaining a small number of faecal samples from consumers and prescribing “personalised” nutritional information for a “healthier microbiome”. However, these initiatives are very controversial given uncertainty in the likely relationships between the gut microbiome, nutrition and various diseases. What these activities do highlight is the demand for such information at a population level. This shows there is an opportunity to improve understanding of the causal role played by the gut microbiome in human health and disease.

Microbiome and variation in our genes
Using information about our genetics can help us find out whether the gut microbiome changes the risk of cancer, or whether cancer changes the gut microbiome. Genetic variation cannot be influenced by the gut microbiome nor disease. Therefore, if people who are genetically predisposed to having a higher abundance of certain bacteria within their gut also have a lower risk of, say, prostate cancer, this would strongly suggest a causal role of those bacteria in prostate cancer development. This approach of using human genetic information to discern correlation from causation is called Mendelian randomization.
Studies relating human genetic variation with the gut microbiome have proliferated in recent years. They have provided evidence for genetic contributions to features of the gut microbiome including the abundance or likelihood of presence (vs. absence) of specific bacteria. This knowledge has given the opportunity to apply Mendelian randomization to better understand the causal impact of gut microbiome variation in health outcomes, including cancer. There are, however, many important caveats and complications to this work. Specifically, there is a (currently unmet) requirement for careful examination of how human genetic variation influences the gut microbiome and interpretation of the causal estimates derived from using Mendelian randomization within this field.
This is exactly what I will be looking at in my new research funded by Cancer Research UK. For more details on the nuances of this work, please see my research feature for Cancer Research UK and paper discussing these complexities.
What’s next for this research?
This research has already shown promise in the application of Mendelian randomization to improve our ability to discern correlation from causation between the gut microbiome and cancer. It has importantly highlighted the need for inter-disciplinary collaboration between population health, genetic and basic sciences. Thus, with the support from my team of experts in microbiology, basic sciences and population health sciences, this Fellowship will set the scene for the integration of human genetics and causal inference methods in population health sciences with microbiome research. This will help us understand the causal role played by the gut microbiome in cancer. Such work acts as a new and important step towards evaluating and prioritising potential treatments or protective factors for cancer prevention.
Acknowledgements
The research conducted as part of this Cancer Research UK Population Research Postdoctoral Fellowship will be supported by the following collaborators: Nicholas Timpson, Caroline Relton, Jeroen Raes, Trevor Lawley, Lindsay Hall and Marc Gunter, and my growing team of interdisciplinary PhD students and postdoctoral researchers. I’d also like to thank the following individuals for comments on this feature: Tom Battram, Laura Corbin, David Hughes, Nicholas Timpson, Lindsey Pike and Philippa Gardom. Additional thanks go to Chloe Russell, a brilliant photographer with whom I collaborated to create “Up Your A-Z” as part of Creative Reactions 2019, who provided the photos for this webpage.
About the author
Dr. Wade’s academic career has focused on the integration of human genetics with population health sciences to improve causality within epidemiological studies. Focusing on relationships across the life-course, her work uses comprehensive longitudinal cohorts, randomized controlled trials and causal inference methods (particularly, Mendelian randomization and recall-by-genotype designs). Kaitlin’s research has focused on understanding the relationships between adiposity and dietary behaviours as risk factors for cardiometabolic diseases and mortality. Having been awarded funding from the Elizabeth Blackwell Institute and Cancer Research UK, Kaitlin’s work uses these methods to understand the causal role played by the human gut microbiome on various health outcomes, such as obesity and cancer. Since pursuing a career in this field, Kaitlin has already led and been key in several fundamental studies that with path the way to resolve – or at least quantify – complex relationships between genetic variation, the gut microbiome and human health. In addition to her research, Kaitlin is actively involved in organising and administering teaching and public engagement activities as well as having many mentorship and supervisory roles within and external to the University of Bristol.
Key publications:
Hughes, D.A., Bacigalupe, R., Wang, J. et al. Genome-wide associations of human gut microbiome variation and implications for causal inference analyses. Nat Microbiol 5, 1079–1087 (2020). https://doi.org/10.1038/s41564-020-0743-8.
Kurilshikov, A., Medina-Gomez, C., Bacigalupe, R. et al. Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat Genet 53, 156–165 (2021). https://doi.org/10.1038/s41588-020-00763-1.
Wade KH and Hall LJ. Improving causality in microbiome research: can human genetic epidemiology help? [version 3; peer review: 2 approved]. Wellcome Open Res 4, 199 (2020). https://doi.org/10.12688/wellcomeopenres.15628.3.
Can lifestyle changes prevent prostate cancer or delay the need for treatment?
 This men’s health week, National Institute for Health Research Biomedical Research Centre and Integrative Cancer Epidemiology Programme PhD student Meda Sandu outlines findings from research on how we can best prevent and treat prostate cancer.
This men’s health week, National Institute for Health Research Biomedical Research Centre and Integrative Cancer Epidemiology Programme PhD student Meda Sandu outlines findings from research on how we can best prevent and treat prostate cancer.
Prostate cancer (PCA) is the second most common cancer in the adult population in the UK, with over 47, 000 new cases being diagnosed each year. Over 400, 000 people assigned male at birth live with or after a diagnosis of PCA. Localised PCA is cancer that is confined in the prostate gland and has not spread to other organs. Localised PCA often grows slowly, may not give any symptoms and/or require treatment. However, occasionally this type of cancer is aggressive in nature, can spread fast and will require treatment. Patients who undergo radical treatment, such as surgery and radiotherapy, often report side effects which significantly impact their wellbeing and enjoyment of life, such as urinary and bowel incontinence, low libido, erectile dysfunction, fatigue, mood swings. Our research looks at lifestyle interventions that may help prevent PCA, as well as identifying cases when treatment may be delayed, in an attempt to best support outcomes for people with PCA.

How does treatment choice affect survival?
In the ProtecT study people were randomised to various treatments or active surveillance where no treatment is given but the patient is regularly followed-up. The study found similar chances of surviving localised PCA, with those in the active surveillance group only having a very small decrease in survival compared to the other groups. This prompted a spur of research in identifying modifiable factors which could delay PCA progression and therefore avoid unnecessary treatment.
One of the aims of our research is to look at dietary and lifestyle changes that are acceptable and achievable to PCA patients, which could reduce PCA risk and progression. These could prevent PCA or, for those who have already been diagnosed with localised disease, delay treatment and therefore avoid the associated side effects.
Dietary and physical activity interventions in people with PCA
In the PrEvENT feasibility randomised controlled trial, patients who underwent prostate removal surgery were randomly assigned to both a dietary and a physical activity intervention. The dietary intervention consisted of either:
- a lycopene supplement, which is an antioxidant found in tomatoes and has been previously be suggested to be protective for PCA
- eating 5 portions of fruit and vegetable per day and replacing dairy milk with a vegan option (soy, almond, oat, coconut etc)
- continue as normal.
The physical activity intervention asked participants to do 30 minutes of brisk walking five times a week.

For each intervention, we looked at the change in metabolites, which are very small molecules found in blood that reflect metabolic patterns, a very useful measure in diseases where there are metabolic changes, such as cancer. We found that eating more fruit and vegetables and decreasing dairy changed blood metabolite levels. Of particular interest was the change in pyruvate levels, a metabolite used as fuel in the pathway of cancer cell proliferation. This suggests that our interventions could lead to less energy being available to the proliferation of cancerous cells, which could lead to lower PCA risk and progression.
Can we predict which PCA cases do not need treatment?
A second aim of my research is to identify blood markers that can help distinguish disease that is unlikely to cause problems from aggressive disease that will advance rapidly and require treatment. We looked at the ProtecT trial and provisionally identified metabolites that could help predict PCA progression. This would allow clinicians to more accurately decide if the patient should take up treatment or if active surveillance would be appropriate.
Patients diagnosed with localised PCA have 96% chance of surviving 15 years after diagnosis. However, PCA risk factors have yet to be conclusively identified. In addition, the diagnosing techniques are invasive and there is uncertainty around which localised cases are likely to advance. More research is therefore needed to establish potential risk factors which could help prevent PCA, and blood-based markers that could predict the aggressiveness of localised PCA cases. We are also looking at the relationship between PCA risk and progression and blood DNA methylation markers, which allow cells to control the expression of genes and have previously been suggested to be responsive to both environmental factors and causes of cancer and could help us better understand the aetiology of PCA.
So what does this mean for people with prostate cancer?
Although more research is required as our studies were small and did not aim to have definitive answers, we did find some evidence to suggest that some lifestyle changes, namely increased fruit and vegetable consumption and replacing milk with non-dairy options and walking 30 minutes a day, 5 times a week are acceptable to PCA patients and that these interventions may have promising effects on blood metabolites. Identifying lifestyle factors which may have a protective role could help prevent PCA cases. Our research also identified metabolites which may help predict the aggressiveness of PCA which could help patients diagnosed with localised PCA avoid serious side effects by not undertaking unnecessary treatment.
Further reading and resources
Find out more about prostate cancer
Find out more about the treatments available for prostate cancer
Journal paper: Hamdy et al (2016) 10 year outcomes after monitoring, surgery, or radiotherapy for localised prostate cancer (the ProtecT trial)
Journal paper: Hackshaw-McGeagh et al (2016) Prostate cancer – evidence of exercise and nutrition trial (PrEvENT): study protocol for a randomised controlled feasibility trial.

