Dr Katharine Looker
‘Enhancing the utilization of COVID-19 testing in schools’, is a study which will look at the characteristics of long COVID and COVID-19 infection in children. ‘Long COVID’ is commonly used to describe signs and symptoms that continue or develop after acute COVID‑19. The study is being funded as a result of a rapid funding call by Health Data Research UK (HDR UK), the Office for National Statistics (ONS) and UK Research and Innovation (UKRI). The study forms part of the larger Data and Connectivity National Core Study, which is led by HDR UK in partnership with ONS.
The COVID-19 testing in schools study is related to the CoMMinS (COVID-19 Mapping and Mitigation in Schools) study being undertaken by the University of Bristol in partnership with Bristol City Council, Public Health England [PHE] and Bristol schools. CoMMinS aims to give us an understanding of COVID-19 infection dynamics centred around school pupils and staff and onward transmission to family contacts, using regular testing. Our study will jointly analyse data from CoMMinS, along with information from Electronic Patient Records, and data from the COVID-19 Schools Infection Survey (SIS; jointly led by the London School of Hygiene & Tropical Medicine [LSHTM], PHE, and ONS). The SIS is a study similar to CoMMinS but carried out nationally.
To help inform research questions and methods for the study, members from the University of Bristol study team gathered views about long COVID in children between 9 March and 30 April 2021 from:
- seven young people from the NIHR Bristol Biomedical Research Centre Young People’s Advisory Group (YPAG)
- five families whose children have long COVID or suspected long COVID, recruited through two online UK campaign groups for long COVID, and
- a survey completed by four GPs and one paediatrician, and an online meeting with two paediatricians.
It is important to note that the opinions gathered were based on small samples which may not be representative.
Through the meeting and survey with the doctors, the study team found that clinical understanding of long COVID in children is currently very limited.
The doctors said that it may be hard to distinguish between long COVID and other conditions with similar symptoms. Many of the symptoms of long COVID, like fatigue and feeling sick, aren’t very specific, and are common to many different conditions. Long COVID in children currently lacks a clinical definition, making diagnosis difficult. It isn’t yet properly understood whether long COVID is a new condition in itself, or a group of conditions like post viral fatigue, which is already recognised.
Young people, and families of children with long COVID or suspected long COVID, who were also asked for their opinion, said that feeling sick or stomach pain, extreme tiredness, and headaches were the symptoms they would rank as most ‘harmful’. For young people, this was based on them imagining having the symptoms. For the families, this was based on their first-hand experience.
The families also said that the symptoms their children were experiencing were numerous, often very severe, and more wide-ranging than those currently listed on the NHS website for long COVID. It is not yet clear what is causing the unusual symptoms.
The families said that they had struggled to get a diagnosis and treatment for their children. They also said that long COVID symptoms were having a significant impact on their children’s day-to-day lives both physically and psychologically, and that some of the children had missed school because of the symptoms. Some of the families also found fevers difficult to manage because their children had to miss school to self-isolate every time they had a fever. They wanted to know why the set of symptoms were being experienced, and why their children in particular had developed them.
It is not known how many children have or will develop long COVID. So far, studies which have tried to measure the rate of long COVID in children suggest it is rare. However, quantifying the number of cases is made difficult by a lack of clinical understanding of long COVID including the lack of an agreed clinical definition. The opinions collected suggest that relying on clinical diagnoses alone will under-estimate cases. On the other hand, there needs to be a cautious approach to estimating the number of cases based on non-specific symptoms, as other conditions which cause similar symptoms may be counted as well.
Caroline Relton, Professor of Epigenetic Epidemiology and Director of the Bristol Population Health Science Institute at the University of Bristol, joint lead for CoMMinS and one of the lead authors of the report, said: “The opinions we gathered further highlight that it is difficult to count the number of children with long COVID on the basis of diagnoses alone while long COVID in children remains poorly defined.
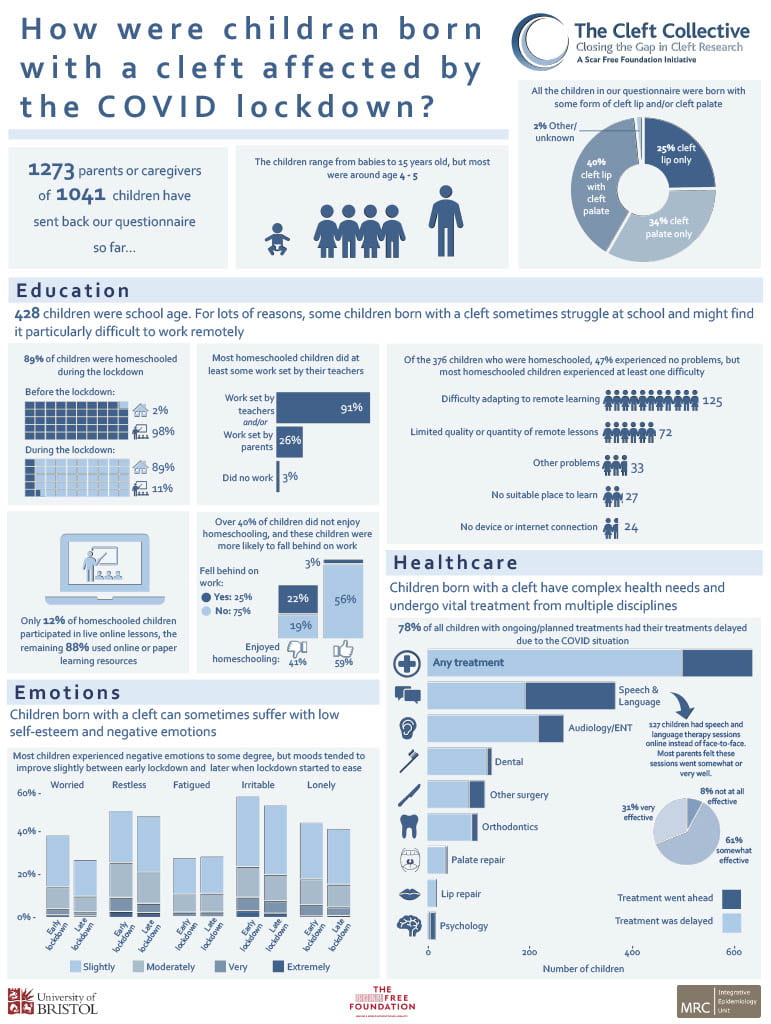
“There are added complications of studying long COVID in children, when it is sometimes difficult to disentangle what might be the result of experiencing infection from what might result from the wider impact of experiencing the pandemic. Isolation, school closures, disrupted education and other influences on family life could all have health consequences. Defining the extent of the problem in children and the root causes will be essential to helping provide the right treatment and to aid the recovery of young people who are suffering.”
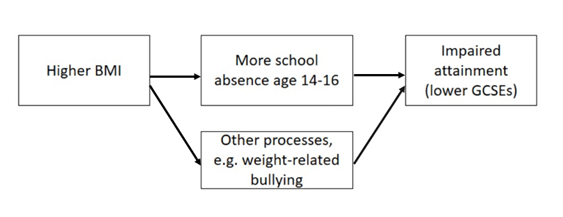
The findings highlight that examining GP and hospital visits, and school attendance, might currently be a more useful and feasible way of assessing how COVID-19 has affected children, rather than relying only on diagnoses of long COVID. However, the study researchers also need to be aware how often healthcare is accessed according to need, and absence from school due to self-isolation, which will affect what is being measured.
Feeling sick or stomach pain, extreme tiredness, and headaches will be important symptoms to consider in the study.
Read the full report
Find the full report on the CoMMinS study news page.