 Alice Carter, PhD researcher at the IEU, outlines the key findings from a paper published in BMJ today.
Alice Carter, PhD researcher at the IEU, outlines the key findings from a paper published in BMJ today.
Heart disease remains the leading cause of death globally, causing over 17.5 million deaths annually. Whilst death rates from heart disease are decreasing in high income countries, the most socioeconomically deprived individuals remain at the greatest risk of developing heart disease. Socioeconomic causes and the wider determinants of health (including living and working conditions, health care services, housing and a number of other wider factors) and are suggested to be the most important driver of health. Behavioural and lifestyle factors, such as smoking, alcohol consumption, diet and exercise, are the second most important contributor to health and disease.
Why does education matter?
Staying in school for longer has been shown to lead to better lifelong health, including reducing the risk of heart disease (cardiovascular disease) and dementia. We also know that those who stay in school are more likely to adopt healthy behaviours. For example, they are less likely to smoke, but more likely to eat a healthy diet and take part in physical activity. These factors, can in turn, reduce the risk of heart disease, such as by reducing body mass index (BMI) or blood pressure. We wanted to understand if these risk factors (BMI, systolic blood pressure and lifetime smoking behaviour) could explain why those who stay in school for longer are less likely to get heart disease, and how much of this effect they explained.
What did we find?
We found that individually, BMI, systolic blood pressure and smoking behaviour explained up to 18%, 27% and 34% of the effect of education on heart disease respectively. When we looked at all three risk factors together, they explain around 40% of the effect. This means that up to 40% of the effect of staying in school reducing the risk of heart disease can be explained by the fact that those who stay in school tend to lead healthier lives. In this work we looked at four outcomes, coronary heart disease (gradual build-up of fatty deposits in arteries), stroke, myocardial infarction (heart attack) and all subtypes of heart disease combined. For all the outcomes we looked at, we found similar results. Notably, the 40% combined effect is smaller than the amount estimated simply from summing the individual effects together. This suggests there is overlap between the three risk factors in how they cause heart disease.
How did we do this?
In our work, we used a few different methods and data sources to answer our questions.
- We started by looking at observational data (that is the data self-reported by the participants of the study) in UK Biobank – a large population cohort study of around 500 000 individuals. Of these, almost 220 000 people were eligible to be in our analysis.
- We looked at how their education affected their risk of four types of heart disease. We then looked at how the intermediate factors, BMI, blood pressure and smoking, could help explain these results.
- Secondly, we replicated these analyses using two types of Mendelian randomisation analyses (a form of genetic instrumental variable analysis, see below), firstly in the UK Biobank group and secondly by using summary data from other studies in the area.
Why use genetic data?
Typically, epidemiologists collect data by asking people to report their behaviours, lifestyle characteristics and any diagnoses from a doctor. Alternatively, people in a study may have been to a clinic where their BMI or blood pressure is measured. However, this type of data can lead to inaccuracies in analyses. This could be because:
- measures are not reported (or measured) accurately. For example, it can be difficult to get an accurate measure of blood pressure, where it changes throughout the day, and even just going to a clinic can result in higher blood pressure.
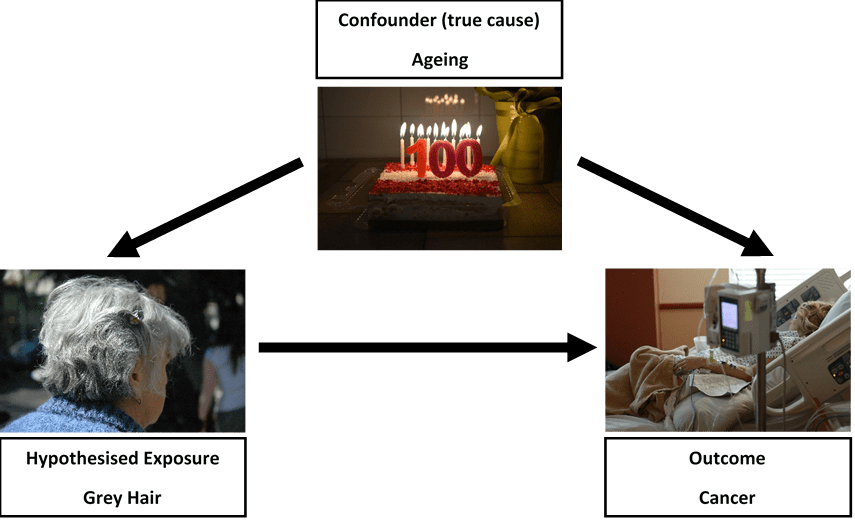
- there may be other variables associated with both the exposure and outcome (confounding). One example of this is suggesting that grey hair causes cancer. Really, age is responsible for i) leading to grey hair and ii) leading to cancer. Without accounting for age, we might suggest a false association exists (see figure 1). In our study using education, this could be ethnicity for example, where it influences both staying in school and risk of heart disease.
- or an individual with ill health may have been advised to change their lifestyle (reverse causality). For example, an individual with a high BMI may have had a heart attack and have been advised by their doctor to lose weight to avoid having a second heart attack.
One way to overcome these limitations is to use Mendelian randomisation. This method uses the genetic variation in an individual’s DNA to help understand causal relationships. Every individual has their own unique genetic make-up, which is determined, and fixed, at the point of conception.
We are interested in single changes to the DNA sequence, called single nucleotide polymorphisms (or SNPs). For all of our risk factors of interest (education, BMI, blood pressure and smoking) there are a number of SNPs that contribute towards the observed measures, that are not influenced by factors later in life. This means, Mendelian randomisation estimates are unlikely to be affected by bias such as confounding, reverse causality or measurement error, as we might expect when we rely on observational data. By using these genetic variants, we can improve our understanding of if, or how, a risk factor truly causes an outcome, or whether it might be spurious.
What else might be important?
Although we find BMI, blood pressure and smoking behaviour explain a very large amount of the effect, over 50% of the effect of education on heart disease is still unknown. In some small sensitivity analyses we looked at the role of diet and exercise as intermediate risk factors; however, these risk factors did not contribute anything beyond the three main risk factors we looked at. Other social factors may be involved. For example, education is linked to higher income and lower levels of workplace stress, but these factors may also be related to those we’ve looked at in this analysis.
One further suggestion for what may be responsible is medication prescribing and subsequent adherence (or compliance). For example, individuals with higher education may be more likely to be prescribed statins (cholesterol lowering drugs) compared to someone who left school earlier, but with the same requirement for medication. Subsequently, of those who are prescribed statins for example, perhaps those with higher education are more likely to take them every day, or as prescribed. We have work ongoing to see whether these factors play a role.
What does this mean for policy?
Past policies that increase the duration of compulsory education have improved health and such endeavours must continue. However, intervening directly in education is difficult to achieve without social and political reforms.
Although we did not directly look at the impact of interventions in this area, our work suggests that by intervening on these three risk factors, we could reduce the number of cases of heart disease attributable to lower levels of education. Public health policy typically aims to improve health by preventing disease across the population. However, perhaps a targeted approach is required to reduce the greatest burden of disease.
In order to achieve maximum reductions in heart disease we now need to i) identify what other intermediate factors may be involved and ii) work to understand how effective interventions could be designed to reduce levels of BMI, blood pressure and smoking in those who leave school earlier. Additionally, our work looked at predominantly European populations, therefore replicating analyses on diverse populations will be important to fully understand the population impact.
We hope this work provides a starting point for considering how we could reduce the burden of heart disease in those most at risk, and work to reduce health inequalities.
Read the full paper in the BMJ
